Diabetic Eye Disease
Imagine pouring flour through a sieve where most it passes through but there are big clumps of flour stuck in the sieve. This is similar to what happens in your body when you have diabetes. As the excess glucose molecules that build up in your body are bigger than your blood cells, they can damage your blood vessels – especially the smaller ones in your toes, fingers, heart and eyes.
Because the effects build up slowly, you may not realise the damage until it’s too late! If you have diabetes, please call us on 3345 3383 to make an appointment for a comprehensive eye test.
What is diabetic eye disease?
There are two main forms of diabetic eye disease: diabetic retinopathy and diabetic macular oedema.
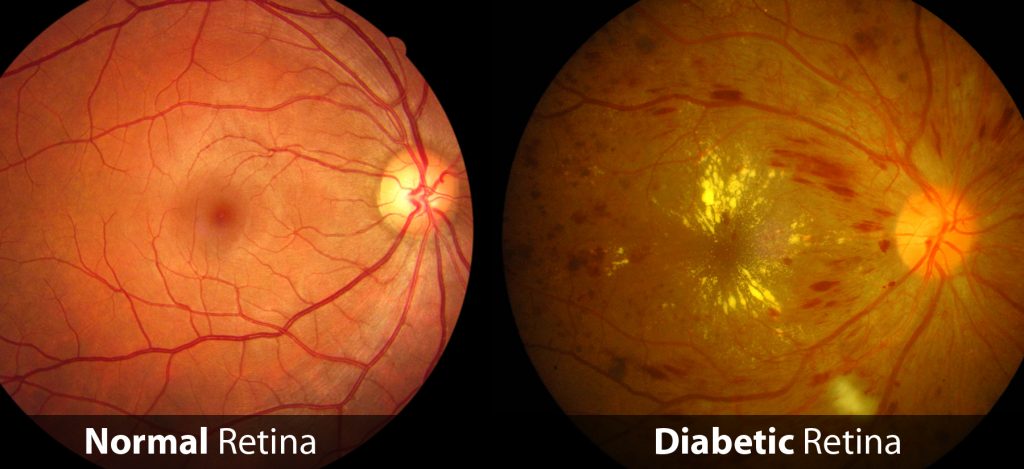
Diabetic retinopathy (DR) is the leading cause of vision impairment and blindness among diabetic working-age adults. Diabetic macular oedema (DME) is a consequence of diabetic retinopathy and is swelling at the macular.
People who are diabetic are also 2-5 times more likely to develop cataracts, and almost at double the risk of developing glaucoma compared with those without diabetes.

Left: Normal vision. Right: Same scene viewed with diabetic retinopathy.
Signs of diabetic eye disease
The early stages of diabetic retinopathy usually have no symptoms and usually progress unnoticed until vision becomes compromised. However common symptoms can include:
- Appearance of ‘floating spots’
- Blurred, distorted vision that can’t be corrected with prescription glasses
- Sensitive to glare
- Difficulty seeing at night time
- Temporary double vision
Many of these symptoms ease when blood glucose levels stabilise.
Risk factors
- Length of diabetes diagnosis. The risk increases the longer a person has diabetes. Women who develop or have diabetes during pregnancy may have rapid development or worsening of diabetic retinopathy.
- Uncontrolled diabetes. The risk increases further if blood glucose levels are not well-controlled as the sugars in the blood will continuously cause damage.
- High blood pressure. The increased blood flow has been hypothesised to damage the small blood cells in the eyes and cause further damage.
Call us on 07 3345 3383 or book online today!
How do I know if I have diabetic eye disease?
Early detection is key!
Diabetic retinopathy can occur regardless of the type of diabetes you have, your age, or even the control you have over your blood-glucose levels. It’s best to have regular eye examinations so that changes can be detected and treated early. It is recommended that those with diabetes should have their eyes checked from when diabetes is first diagnosed, and then regularly checked every year after that.
We offer professional testing using a combination of the following techniques:
- Tonometry to measure pressure inside the eye
- Pupil dilation using eye drops helps to give a better view of the retina and optic nerve at the back of the eye. This also includes digital photos of your retina. This requires a longer appointment approx. 45mins.
- OCT imaging is a non-invasive ultrasound scan of the multiple layers underneath the retina. It allows accurate diagnosis of any swelling at the macula, and also provides early detection a variety of other eye diseases.
View our OCT scanning equipment.
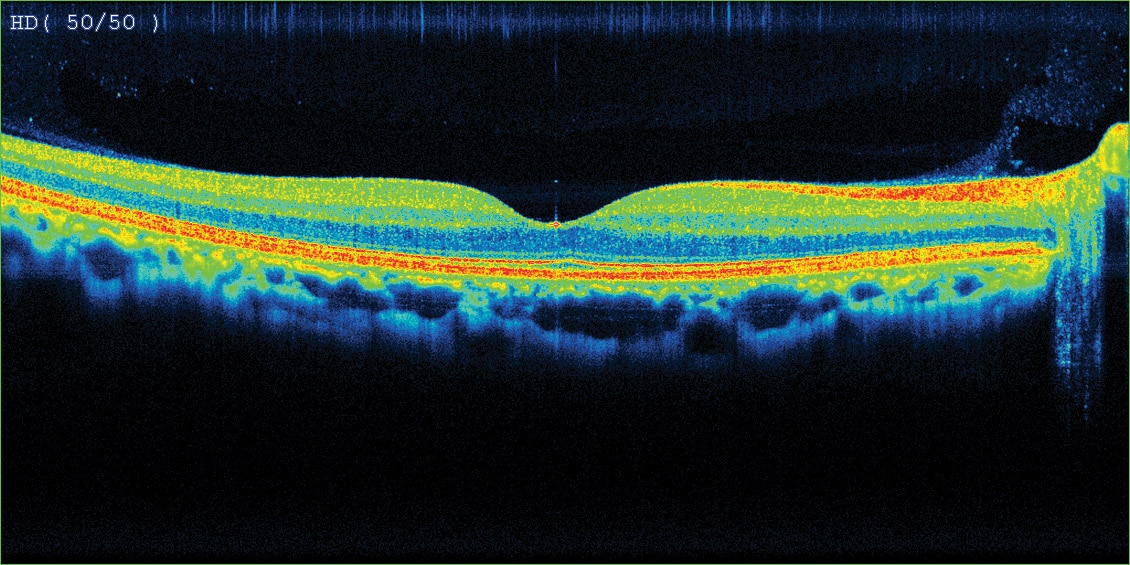
Left: OCT scan of normal macula
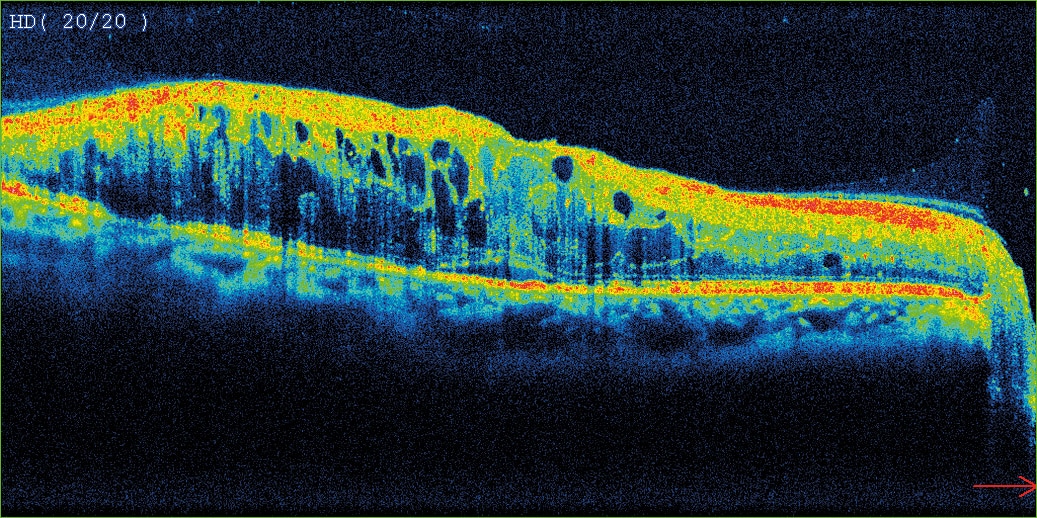
Right: OCT scan of diabetic macular oedema
Prevention
- Control blood glucose levels either through diet or a doctor-prescribed insulin regimen.
- Regular exercise 20 minutes a day, 5 days a week.
Regular exercise at all ages improves balance, strength, mobility and reaction time, and can reduce the risk of injury in the event of a fall. In terms of diabetes, it helps your body absorb excess glucose. It can also help to manage chronic conditions such as arthritis, depression and high blood pressure. - Nutrition plays an important role in controlling diabetes, although a healthy, well-balanced diet is good for overall wellbeing as well. Some general tips are:
- Have a diet that aligns with Queensland Health’s ‘Healthy Eating Guidelines’ and ‘Australian Guide to Healthy Eating’
- Limit intake of unhealthy fats and oils
- Eat a variety of fresh fruit and vegetables everyday
- Have a consistent distribution of low GI carbohydrates throughout the day
- Consult a dietitian for an in-depth analysis of your diet and individual recommendations.
Treatment options
- Laser treatment seals leaking blood vessels which helps to prevent vision loss.
- Intra-vitreal Anti-VEGF injection treatments are also used to slow down new blood vessel growth and stop leakages in cases where DME is present. Ophthalmologists may also consider intra-vitreal steroid injections.
- Surgery may be required for severe cases of diabetic retinopathy.
Please feel free to make an appointment on 3345 3383 for a detailed assessment and specialist referral.