Glaucoma
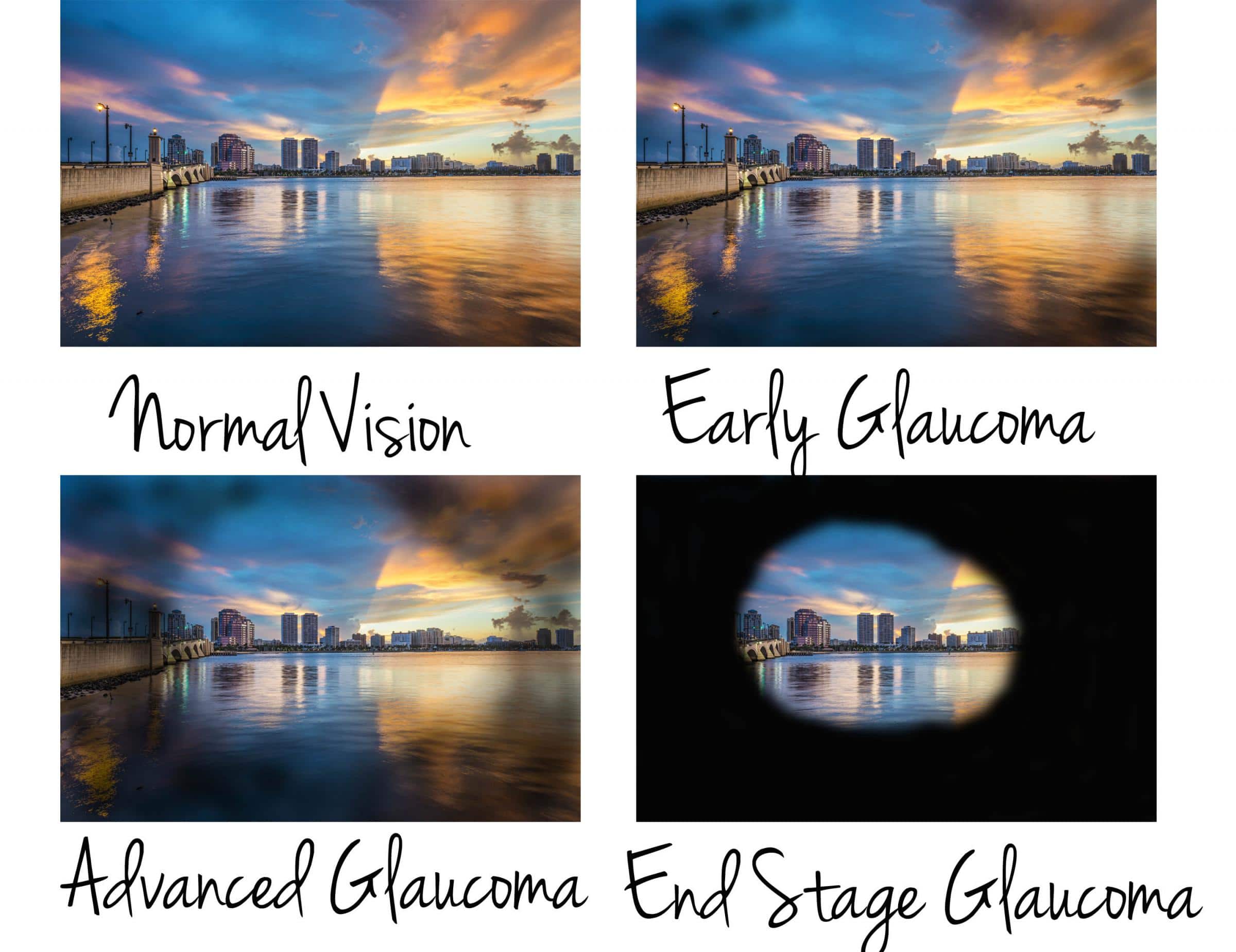
Glaucoma is known as the “silent thief of sight” because a condition that generally does not exhibit any symptoms or warning signs until significant vision loss has occurred. It is a condition which results in a progressive and painless loss of side vision due to damage to the optic nerve, which is responsible for carrying the messages from our eyes to the brain.
If you are worried about glaucoma, call (07) 3345 3383 to book a comprehensive assessment!
Types of glaucoma
Open-angle glaucoma
- Most common type, accounting for at least 90% of all cases
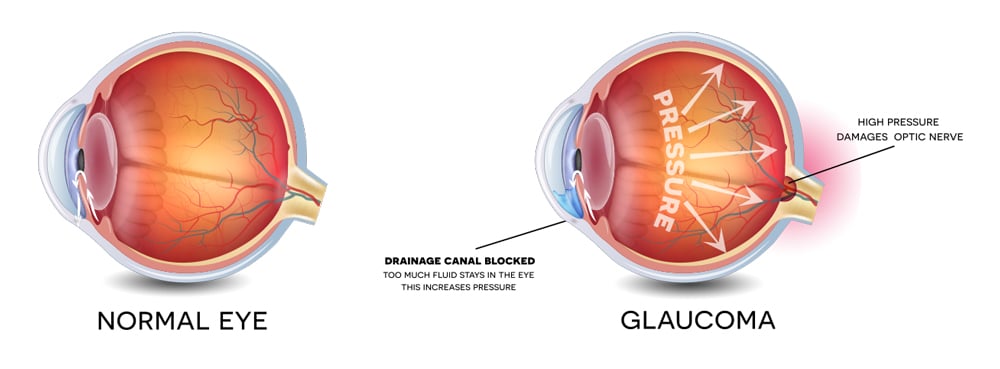
- Caused by slow clogging of drainage canals = slow increase in eye pressure
- Develops slowly and is a lifelong condition
- Symptoms are often not noticeable until very severe
Angle-closure glaucoma
- Caused by blocked drainage canals = sudden increase in eye pressure
- Develops quickly and needs immediate attention
- Symptoms are noticeable
Normal-tension glaucoma
- Optic nerve is damaged = unchanged eye pressure
Congenital glaucoma
- Due to incorrect or incomplete development of the eye’s drainage system
Signs of glaucoma
The signs of glaucoma are generally quite subtle and hard to detect. This is why it is so important to have regular eye checkups by an eye care professional, especially if you are at a higher risk. The only way to check if you have glaucoma is to visit an optometrist for a full eye examination.
In cases of angle-closure or severe open angle glaucoma, the most noticeable symptoms are:
- Hazy or blurred vision
- Appearance of rainbow-coloured circles around bright lights
- Severe eye and head pain
- Nausea or vomiting
- Sudden vision loss
Risk factors
Glaucoma is caused by both genetic and environmental factors:
- Family History. In many cases, glaucoma is passed on within families and the risk increases with direct relatives. 1 in 4 direct relatives may develop glaucoma in their lifetime. Therefore it is very important for family members of those people with glaucoma to undergo a glaucoma eye examination.
- High eye pressure. People with glaucoma often have higher eye pressure than normal.
- Age. Those over the age of 50 are at higher risk.
- African or Asian descent.
- Diabetes increases the risk of developing glaucoma by almost double.
- Short sightedness. The stretching of the eyeball that occurs in people with short sightedness may damage the optic nerve and thus increase the risk of glaucoma.
- History of eye injury.
- Past or present prolonged use of steroids.
- Migraine
- High or low blood pressure
- Sleep apnoea.
Call us on 07 3345 3383 or book online today!
How does Glaucoma cause vision loss?
Early detection
The earlier a diagnosis is made, the earlier steps can be taken to slow disease progression. Delayed treatment can increase the likelihood of losing sight.
We are equipped with state of the art instruments on top of the standard eye examination procedures:
- Eye pressure measurements provide information regarding the risk of developing glaucoma.
- Anterior chamber angle assessment helps determine if the drainage pathway for the fluid leaving the eyeball is narrow or blocked. If this angle is narrow, this will lead to fluid build up and subsequently higher eye pressure.
- Digital retinal photographs provide a detailed image of the optic nerve head and give a baseline for comparison for future eye exams. In glaucoma, the optic nerve head will appear excavated. This comes free with our comprehensive eye examinations.
- Visual field test provides a formal assessment of the sensitivity of your side vision. This test is subjective and may take a few repeated tests to determine the most accurate result.
- OCT imaging is a non-invasive ultrasound scan to assess the thickness of the nerve fibres supplying the optic nerve head (retinal nerve fibre layer). In glaucoma, the RNFL becomes thinned. The OCT imaging provides earlier detection of nerve damage compared to visual field tests.
- Glaucoma and Macular degeneration assessment package. This includes a visual field test (detects early signs of glaucoma), dilated eye examination, 3D digital retinal photographs, and OCT scan.
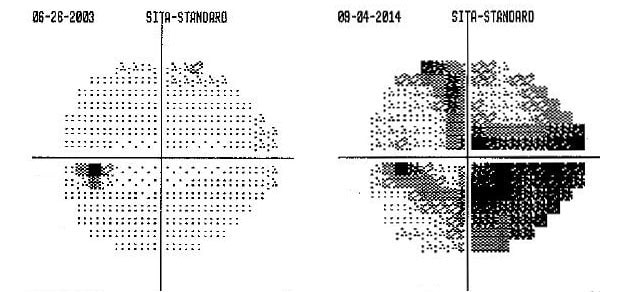
Left: Normal visual field. The black spot on the left side is the normal “blind spot”. Right: Abnormal visual field showing reduced vision in both central and peripheral areas.
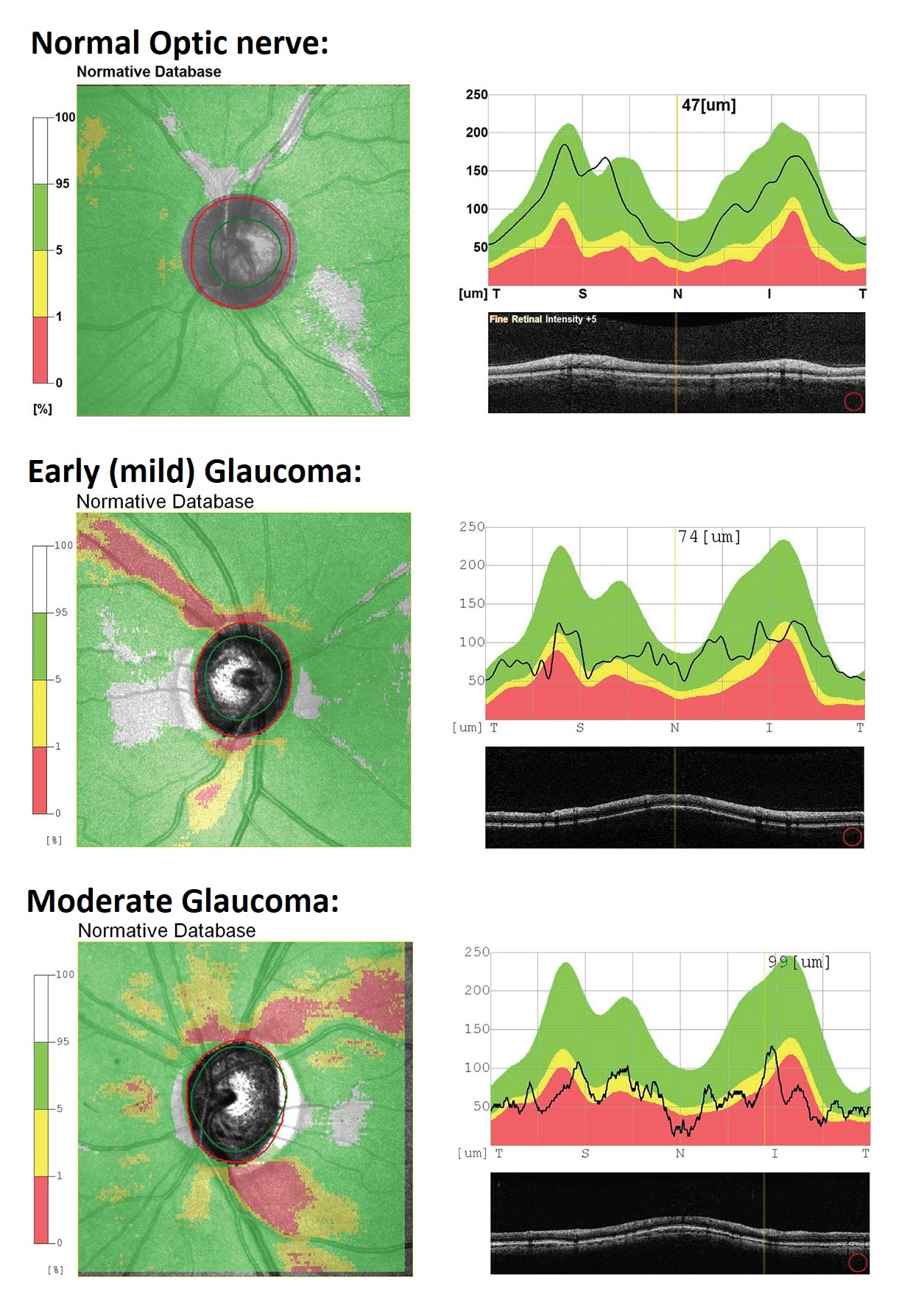
Glaucoma progression as measured with an OCT
Reducing your risk of glaucoma
- Nutrition plays an important role in optimising eye health. A healthy, balanced diet is good for overall wellbeing as well as eye health.
- Have a diet that aligns with Queensland Health’s ‘Healthy Eating Guidelines’ and ‘Australian Guide to Healthy Eating’
- Limit intake of fats and oils
- Eat dark green, leafy vegetables and fresh fruit daily
- Eat fish two to three times a week
- Choose low GI carbohydrates
- Eat a handful of nuts a week
- Red wine also helps to provide extra anti-oxidants and temporarily reduces eye pressure.
- Consult a dietitian for more information on your nutritional needs
- Regular exercise 20 minutes a day, 5 days a week.
Regular exercise at all ages improves balance, strength, mobility and reaction time, and can reduce the risk of injury in the event of a fall. In terms of glaucoma, exercise helps to reduce eye pressure, and also maintain the health of all blood vessels. Physical activity can also help to manage chronic conditions such as arthritis, diabetes, depression and high blood pressure. - Stop smoking
- Ensure normal blood pressure and cholesterol levels
- Control diabetes




Treatment options
Although the side vision loss is not reversible, early detection and treatment will be effective in controlling the progression of any further vision deterioration. The treatment option will depend on whether you have ‘open angle glaucoma’ or ‘angle closure glaucoma’.
Please note that this is general advice only – please consult your ophthalmologist for more information.
- The first step in treating glaucoma is to treat any underlying condition that is causing the glaucoma.
- Eye drops. Most people with glaucoma are able to successfully manage their condition with the use of ophthalmologist-prescribed eye drops. Remember – drops can only work if you use them correctly.
- Oral medication may be used to treat open-angle glaucoma, however it is usually only used for a short time as its effectiveness can reduce over time.
- Laser treatment may be performed in some cases of glaucoma to allow improved fluid flow within the eye.
- Surgery may be necessary when laser treatments are not successful.
Living with glaucoma
- Continue with your daily activities. Using your eyes is not harmful and they do not need to be “rested”. Reading, writing, sewing, computer work and similar activities encourage your eyes to focus up close. This exercises the muscles in and around your eyes which helps excess fluid to drain more effectively and eye pressure to fall. Similarly, longer distance viewing such as driving or watching TV will not harm your eyes.
- Whether you are fit for driving depends on the amount of vision loss your glaucoma has caused. The legal visual acuity required for driving in Australia is 6/12 or better, with both eyes open. There also needs to be at least 120 degrees of visual field free of glaucoma defects. This can all be assessed with your optometrist.
- Sleeping position. There is some evidence that sleeping with physical pressure on the eye can accelerate damage related to glaucoma. Therefore it is recommended to avoid sleeping in positions where physical pressure or strain is put on the eyes.
- Physical exercises to avoid
- Yoga: where your head is held below the waist, such as “downward dog”.
- Swimming with goggles. Swimming goggles have been linked to increased eye pressure. Choose goggles that fit snugly to the bones around the eyes, and do not apply pressure to the eye balls.
- Weight lifting. Try to breathe in as you lift the weights – don’t hold your breath. This avoids strain and pressure building up in the veins of your head, neck and eyes. Try to choose more repetitions with lighter weights, rather than few lifts with heavier weights.
- Wind instruments. The excessive pressure exerted when playing can elevate eye pressure.
- Depression and social withdrawal is common in patients with advanced glaucoma, and is associated with reduced quality of life. If you or someone you know is experiencing depression or anxiety due to your experience with vision loss, please speak to your doctor of health care professional.
If you are worried about glaucoma, call (07) 3345 3383 to book a comprehensive assessment!